Relief from Menstrual Pain
Shark week. The crimson tide. Riding the cotton pony. The many, creative terms we have for periods offer little comfort when it’s time for dealing with the unpleasantries that accompany it.
Although menstruation is a perfectly normal cyclical process for the female body, it can cause discomfort. Cramping, aching, and a dull heaviness in the lower abdomen are common. There are many different ways to reduce period pain, but before taking action it’s important to understand what hurts and why.
Abdominal pain during “Code Red” is sometimes accompanied by lower back pain that can extend down through the legs. You may also experience nausea, vomiting, headaches, and diarrhea, and you may feel irritable or fatigued. Although less common, some women also feel dizzy and can faint. Menstrual pain can impede even the most routine activities for 1–3 days each month, so this may not be the best time for intense physical activity, competitions, or long hikes. On the other hand, some women experience very mild pain or no symptoms at all. It depends on the characteristics of each woman’s body and on her overall health.
Not pregnant? Here comes your period…
Even if you aren’t thinking about having children or starting a family, but want to study, build your career, or enjoy your hobbies, your body will nevertheless prepare for pregnancy every month. The mucous membrane that lines the uterine cavity—the endometrium—gradually thickens so a fertilized egg cell can nestle into it safely and comfortably.
If an egg cell isn’t fertilized, the endometrial lining gradually sheds away. Period pain is due to muscle contractions caused by biologically active lipids called prostaglandins. Contractions push blood and endometrium from the uterus. The more prostaglandins there are in the body, the more powerful the contractions and the more discomfort you will feel; powerful contractions can block adjacent arteries, inhibiting oxygen supply to the uterus and causing pain.
You may start to feel pain 1–3 days before menstruation begins. During this time the pain is generally dull and continuous. The pain is usually most intense during the first two hours of menstruation and can last for up to three days.
Studies show that menstruation is most painful for women aged 23–27.
Extreme menstrual pain caused by excessive levels of prostaglandins is called dysmenorrhea. This condition can afflict young women just beginning to menstruate (primary dysmenorrhea) but older women who may never have had painful periods before can also experience this (secondary dysmenorrhea). In an older woman, dysmenorrhea may be caused by a more serious condition, such as endometriosis (endometriotic tissue growing where it shouldn’t), ovarian cysts, or myoma (a benign uterine tumor). Therefore, talking to your gynaecologist is highly recommended. Diagnosis and treatment can drastically reduce period pain.
Other culprits
There can be other reasons for painful periods as well, such as anatomical peculiarities (a narrow uterine opening or a tilted or retroverted uterus), excess weight, smoking or drinking, an irregular menstrual cycle, starting to menstruate early (before age 11), prolonged periods of stress, excessive or unusual physical exertion, or an emotional ordeal such as the loss of a loved one, relationship problems, or heartbreak.
Periods tend to be most painful for women who are not yet sexually active and for women who haven’t given birth.
Once a woman has gone through pregnancy and labour, period pain tends to diminish or disappear entirely due to physiological changes in the uterus and cervix. Genetics can also play a significant role—if a woman has had intense and painful periods it’s very likely that her daughter will have a similar experience. Period pain may also be related to diet—coffee and other caffeinated drinks, and too many spicy, salty, or sweet foods can increase the amount of pain your experience.
Find what works best for you
There is no single magic pill that can take the discomfort away for everyone. The methods are as different as women are themselves. One might only need an extra hour of rest, another will swear by meditation or yoga, another might only find refuge in painkillers. The only universal recommendation for dealing with your “moon time” is to treat yourself well—don’t overwork yourself, get plenty of sleep, eat healthily, hydrate, try not to stress, and don’t overdo physical activities.
Other suggestions:
- If you experience severe menstrual pain, a good option may be to ask your family doctor or gynaecologist to recommend appropriate painkillers. If your menstrual pain is predictable, take them as soon as it begins or even a little beforehand as no medication works instantaneously.
- Milder treatments include dietary supplements (vitamins, omega-3 fatty acids), herbal preparations, and homeopathic medicine—these can successfully reduce discomfort for some women. Talk to a doctor or homeopath for suggestions.
- Certain herbal teas can also help but note that they’re effective only after extended regular use.
Medical opinions on using heat differ. Some doctors advise against it, because heat can increase bleeding, but others recommend warm baths, or a hot water bottle applied to the abdomen for the relaxing effect.
- Kinesiology tape placed on the lower abdomen and back can also help. For best results, visit a physiotherapist for application a day or two before your period.
- Acupuncture or dry needling can prove effective for women who favour alternative methods.
- If your menstrual pain is caused by illness or disease you must seek diagnosis and treatment. Ultrasound or other diagnostic imaging are common techniques, and in some cases laparoscopy is used. If a myoma or ovarian cyst is discovered, surgery may be required.
- Taking into consideration your overall health, age, needs, and habits, your gynaecologist may recommend hormonal contraceptives, such as birth control pills or a hormonal IUD, to treat dysmenorrhea—this can help in cases of hormone imbalance.
- Certain positions also relieve pain, such as the foetal position: lie on your side or back with your legs pulled up to your stomach. Getting down on all fours can also help relieve pain. You can lightly massage your abdomen and lower back yourself or ask a friend or partner to do it for you, but make sure to ask them to be gentle.
- A light, but nutritious and vitamin-rich diet is recommended during menstruation—for example rolled oats, bananas, walnuts, a variety greens, ginger, and sunflower seeds.
- If you have enough strength and energy reserves, do some moderate physical exercise such as yoga, jogging, or a gentle workout with plenty of stretching. Making physical activity a part of your normal routine is important for reducing menstrual pain and for your overall health.
Attention! If you are experiencing severe pain accompanied by elevated temperature and other atypical symptoms associated with infections, or you have never experienced similarly strong menstrual pain, or if your period pain comes on suddenly and is accompanied by intense bleeding, this should be considered an emergency. Seek medical help without delay!
Visiting your doctor
If you are having difficulty managing period pain, visit your doctor or gynaecologist. Prepare beforehand. You will likely be asked the following questions: How old were you when you first got your period? When was your last period? Is your cycle regular? How long is it? Do you experience bleeding or “spotting” between periods?
Your gynaecologist will probably also ask you about your mother’s experiences and your family’s medical history. If you don't know, ask. Remember to tell your doctor what treatments you have tried so far and how effective they’ve been. Other relevant information includes recent illnesses, any medications or dietary supplements you use, recent emotional ordeals, and other stressors in your life.
You may be asked about your sex life - whether or not you are sexually active and if you experience pain during intercourse.
Don’t be afraid to ask questions, for example: What are potential sources of my period pain? How likely is it that I can reduce or eliminate the pain? What examinations or analyses will be necessary? What medicines or alternative treatments are best suited for me?
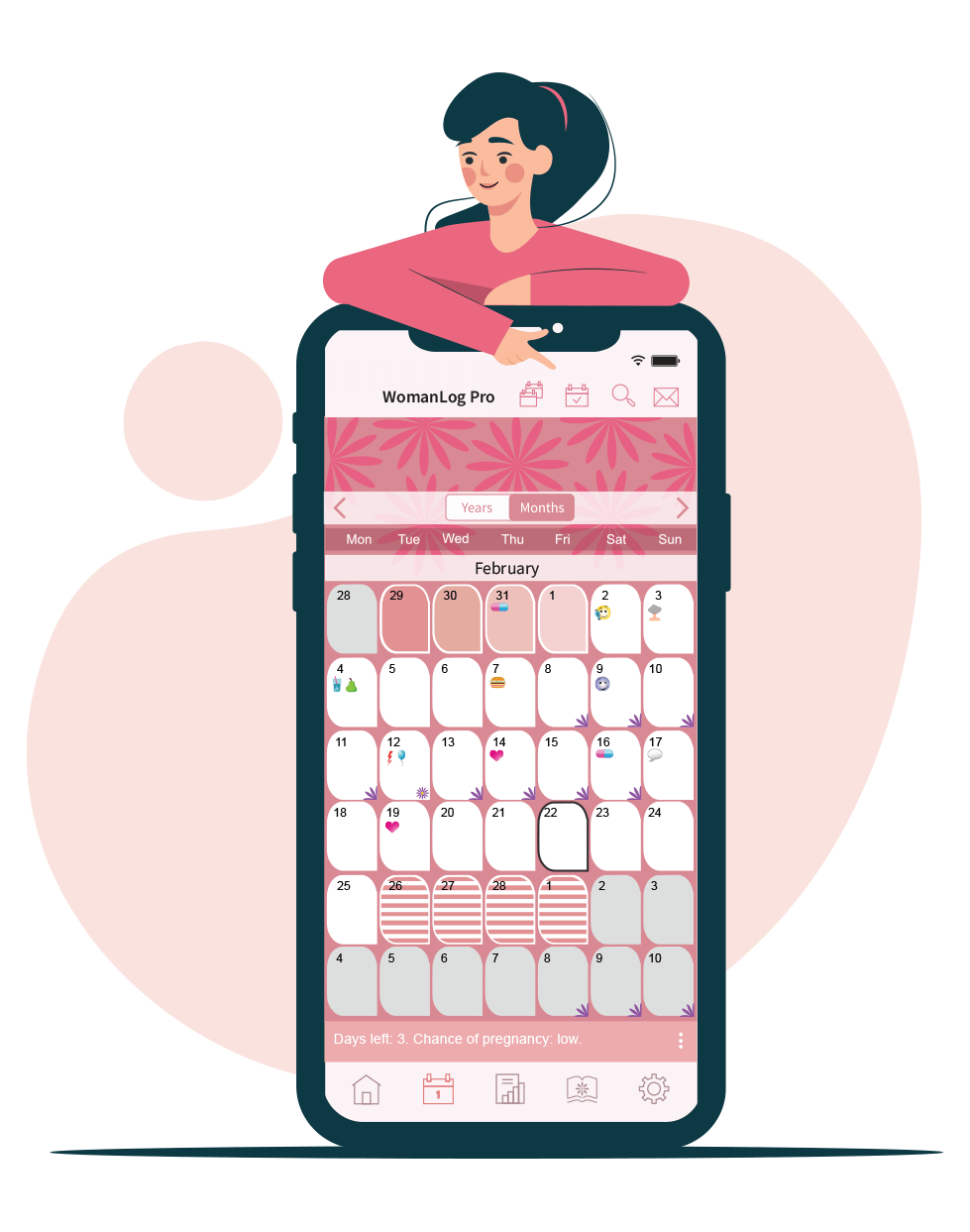
You can track symptoms using WomanLog. WomanLog has more than 100 symptoms. Download WomanLog now: